Negligent Management of Fetal Distress
Our firm represents children and parents who have been injured due to negligent management of fetal distress.
What is fetal distress?
Fetal distress is a condition in which a fetus experiences difficulty during labor and delivery. It is a potentially life-threatening situation for both the mother and the baby, and requires prompt recognition and intervention by medical providers. In this article, we will discuss the various signs and symptoms of fetal distress, as well as the appropriate actions that medical providers should take in order to properly diagnose and manage this condition.
How do medical providers recognize fetal distress?
Labor and delivery doctors and nurses are required to know the signs and symptoms associated with fetal distress. These may include changes in the fetal heart rate, such as a decrease in the fetal heart rate or an abnormal pattern of decelerations. Other signs may include decreased fetal movement, or a change in the fetus's position, such as a breech presentation. Additionally, the mother may experience a change in her own vital signs, such as an increase in blood pressure or decreased oxygen saturation.
ACOG (The American College of Obstetricians and Gynecologists) recommends that healthcare providers assess fetal well-being during labor and delivery by monitoring the fetal heart rate and pattern. This involves using ultrasound or electronic fetal monitoring (EFM) to measure the fetal heart rate and detect any changes in the fetal heart rate pattern. The EFM provides a continuous record of the fetal heart rate, allowing medical providers to identify any concerning patterns, such as reduced heart rate variability or heart rate decelerations, which can indicate that the baby is in distress.
Careful attention to EFM charting, combined with proper assessment of mother and baby, should result in medical providers recognizing if a baby is in distress.
How should medical providers respond to data from EFM charting?
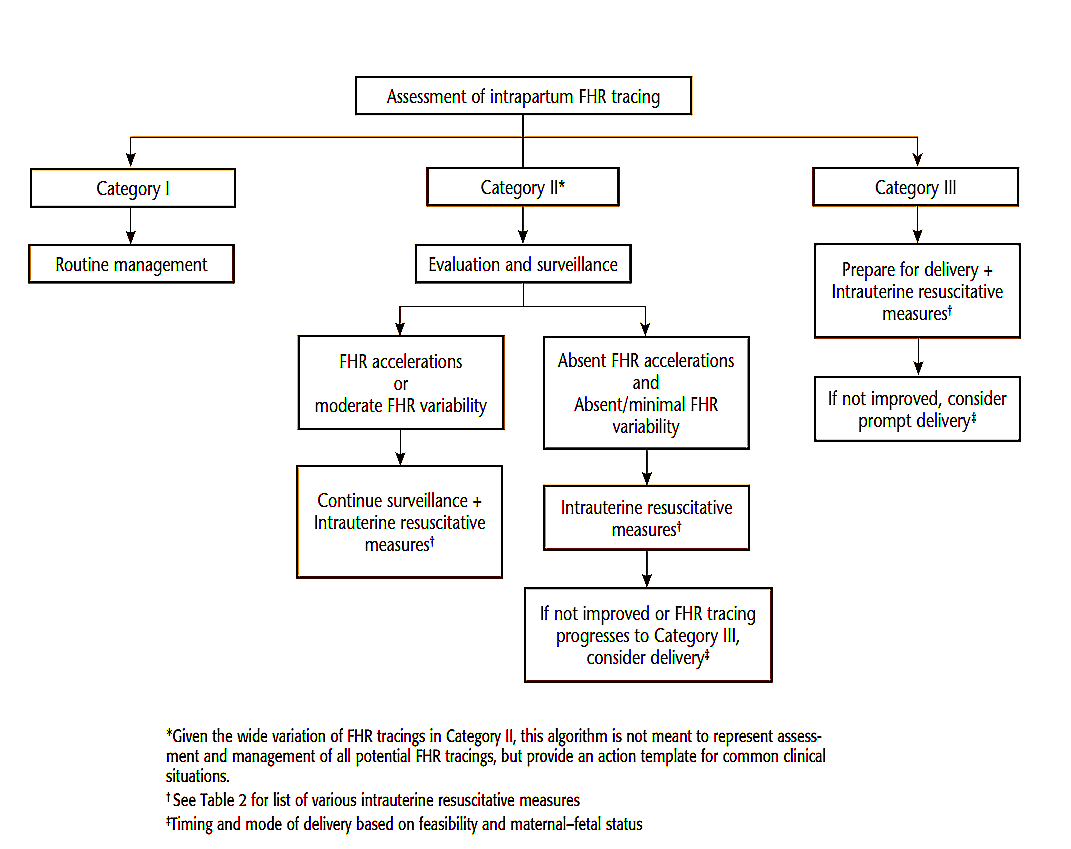
ACOG Practice Bulletin No. 116: Management of Intrapartum Fetal Heart Rate Tracings provides guidance on the management of abnormal fetal heart rate (FHR) tracings during labor. The bulletin emphasizes the importance of a systematic approach to FHR monitoring and management, with appropriate intervention to prevent adverse outcomes.
The bulletin outlines a three-tier classification system for FHR patterns: Category I, II, and III (discussed in greater detail below). Category I tracings are considered normal, while Category II tracings are indeterminate and require further evaluation. Category III tracings require immediate resuscitative measures and preparation for delivery. ACOG Practice Bulletin No. 116 sets forth the following treatment algorithm:
What is the standard of care when a fetal heart rate pattern is unclear or indeterminate?
When a baby's fetal heart rate (FHR) pattern deviates from normal, the healthcare provider must immediately take steps to further evaluate fetal well-being. Failure to do so constitutes negligence by the provider.
Under ACOG's classification system of FHR patterns, any indeterminate FHR pattern is deemed a "Category II" tracing. A Category II tracing literally means there is not adequate evidence to know whether a fetus is in distress. In the absence of such evidence, it is unacceptable to proceed with normal management of labor. Instead, providers should urgently gather additional information for further evaluation and possible intervention. This may involve additional fetal monitoring, fetal scalp stimulation, or fetal blood sampling. Interventions may be undertaken to optimize maternal and fetal oxygenation, such as changing the mother's position or providing oxygen supplementation.
In situations where the cause of the distress is not apparent, medical providers may need to take more aggressive measures to manage the situation. This may include providing the baby with oxygen through a procedure called fetal scalp electrode, or delivering the baby through an emergency cesarean section.
Careful additional analysis of the FHR tracings must be undertaken to determine the baby's status. Based on those findings, providers should consider appropriate resuscitative measures. If the baby's status still does not improve, the fetal health status is considered "Category III" and immediate delivery should be considered.
What is the standard of care once fetal distress is apparent?
Once fetal distress has been identified, medical providers must take immediate action to manage the situation. A fetal heart rate pattern that is abnormal and indicates possible fetal distress is classified by ACOG as "Category III" tracing. Abnormal patterns that indicate fetal distress include but are not limited to:
- Absent variability with recurrent late decelerations, recurrent variable decelerations, or bradycardia
- Sinusoidal pattern (a smooth, undulating pattern in the fetal heart rate)
According to the guidelines established by the National Institute of Child Health and Human Development (NICHD), a Category III FHR tracing requires prompt evaluation and management. In other words, once a Category III FHR tracing is identified, the healthcare provider must take prompt action to evaluate fetal well-being and may need to consider delivery if the fetus is at risk of harm.
The healthcare provider will typically take steps to further evaluate fetal well-being, which may include additional fetal monitoring, fetal scalp stimulation, or fetal blood sampling. They may also consider interventions to optimize maternal and fetal oxygenation, such as changing the mother's position or providing oxygen supplementation.
The first step is to try to determine the cause of the distress. This may involve performing additional tests or procedures, such as amniocentesis or cordocentesis, to measure the oxygen levels in the fetus. Other interventions may include changing the mother's position or attempting to deliver the baby by cesarean section. In general, mild fetal distress may not require immediate intervention, while more severe distress may require prompt delivery to prevent harm to the fetus.
Contact a Kentucky birth injury attorney with experience handling fetal distress cases.
Understanding FHR tracings and other aspects of fetal distress is complex and requires specialized training and experience. For this reason, if you or a loved one have been injured due to medical care received during labor and delivery, it is important to speak to an experienced birth injury attorney.
From our offices in Louisville, Kentucky, Powell Klausing represents families across the region on cases involving complex birth injuries. We have access to a team of medical experts who can help determine whether your labor and delivery should have been managed differently. We will gladly listen to your story and provide a complimentary analysis as to whether further investigation is warranted. Give us a call today for a free consultation.
Related:
- ACOG Practice Bulletin No. 106: Intrapartum Fetal Heart Rate Monitoring: Nomenclature, Interpretation, and General Management Principles. This practice bulletin provides an overview of FHR monitoring, including the classification system for FHR patterns and the general principles of FHR interpretation and management
- ACOG Practice Bulletin No. 116: Management of Intrapartum Fetal Heart Rate Tracings. This practice bulletin provides specific guidance on the management of abnormal FHR tracings, including Category II and Category III tracings.
- ACOG Committee Opinion No. 684: Disclosure and Discussion of Adverse Events. This committee opinion emphasizes the importance of communication and disclosure in cases of adverse events, including those related to fetal distress and birth trauma.
- ACOG Committee Opinion No. 767: Emergent Therapy for Acute-Onset, Severe Hypertension During Pregnancy and the Postpartum Period. This committee opinion addresses the management of hypertensive emergencies during pregnancy and the postpartum period, which can be a contributing factor to fetal distress.
